
For around 2.5 million people worldwide with multiple sclerosis (MS), coping with aching, stiff, spastic and cramping muscles is something they deal with all the time. And, another 15 million individuals with spinal cord injuries are suffering from many of the same symptoms — pain, muscle stiffness, sleep problems and spasticity.
While traditional treatments can help reduce their pain and discomfort, they may not experience total relief. Plus, the medications cause adverse and intolerable side effects like drowsiness, weakness, nausea, and others.
Because of this, it’s no surprise many patients are turning to cannabis to find relief. Since muscle spasms are a common symptom among almost all these patients, researchers are studying and testing medical cannabis for spasticity as an alternative treatment for this highly uncomfortable symptom.
Spasticity is where your muscles contract continuously. The contraction causes muscle tightness and stiffness interfering with walking and normal movement. Spasticity typically occurs due to damage to the area around your spinal cord and brain that controls voluntary movement. You then experience a change in the balance of your muscles and nervous system signals, leading to increased muscle activity. Spasticity affects your joints and muscles negatively.
When experiencing spasticity, it could feel like a mild tightness sensation in your muscles, or it could cause you severe, uncontrollable and painful spasms of your extremities — usually in the arms and legs. Spasticity can also cause lower back pain and tightness and pain in and around your joints.
Symptoms of spasticity usually include:
Symptoms often occurring with MS spasticity and spasms include weakness, pain and rhythmic contractions known as clonus.
Spasticity may affect any of your body’s muscles, depending on where in your spinal cord and brain it affects nerves. Spasticity can occur due to the following reasons.
Muscle tone increase: An increase in your muscle tone can cause spasms and spasticity. Your muscle tone is the degree of resistance or tension to muscle movement. Muscle tone allows you to hold a position or move your limbs.
Nerve signal damage: Your nerve pathways connecting your spinal cord, muscles and brain work simultaneously to coordinate smooth movement. If MS-related damage interrupts your brain and muscle nerve signals, your muscle could stay in its shortened state, making your affected limb feel tight, stiff and hard to move.
When you have a limb remaining in one position, it’s called a contracture. When there’s disruption to the nerve messages, it can also cause muscle overactivity and coordination loss leading to spasms.
Other ailments: Several other conditions can cause spasticity, including the following.
You can have spasticity depending on these types of underlying conditions.
Spasticity usually affects the muscles you need to support an upright standing position, like those of your:
You can also develop extensor spasticity where your legs straighten involuntarily. Your front, upper leg muscles known as your quadriceps are usually involved with extensor spasticity, alongside your inner thigh muscles, or adductors. The knees and hips stay straight with the leg crossed over at your ankles or extremely close together. You may also experience spasticity in your arms. However, this is not as common in MS patients.
Certain factors can aggravate the problem. For instance, a bladder infection left untreated could contribute to spasticity.
Mild spasticity could interfere with proper motion, affect how you walk or it could take more effort for you to move, and it could limit how far you’re able to go. Severe spasticity could cause certain degrees of disability and could be painful. In some cases, you may still be able to walk with certain degrees of spasticity, even with weak leg muscles.
If your doctor doesn’t treat spasticity, permanent shortening of tendons and muscles could make your joint seize up — referred to as joint contractures. Joint contractures could painfully deform your joints and could make it hard for you to eat, communicate and perform many of your daily tasks. There’s a way to control spasticity, fortunately, so you can still perform many of your daily activities.
One study reported by the Multiple Sclerosis Society of America found spasticity had a direct effect on a person’s quality of life in the presence of certain variables like:
As the spasticity in an individual becomes more severe, their overall quality of life worsens significantly.
The study also found spasticity could negatively affect a person’s social roles and psychological health. It can affect employment, relationships and future planning. Study participants reported spasticity affects their depression, anxiety, controlling abilities and low self-esteem. Along with depression, researchers found a strong association between spasticity and pain, fatigue and bladder dysfunction.
Facts about spasticity, according to the American Association of Neurological Surgeons, include:

While Hippocrates already used the Greek word spasmos to describe an epileptic fit, only in more recent literature has there been the use of the term spasticity. A physician named John Mason Good used the term in English in 1829. He described “spastic wryneck: from an excess of muscular action on the contracted side.” By that time, the use of the term was similar to what it is today.
Several treatments for spasticity exist, but your doctor needs to evaluate treatment options on an individual basis, depending on how old you are, what the underlying cause of your spasticity is and how severe it is. Treatments may include the following.
Your doctor may prescribe oral medications when your spasticity symptoms are interfering with your everyday functioning or affecting your sleep. Your doctor may prescribe a combination of medications, or they may prescribe medication with another form of treatment, such as surgery.
You’ll need to work closely with your doctor to come up with an individualized treatment plan. Each medication will have a different set of side effects.
Here are the most common prescription drugs for spasticity.
Botox used in tiny amounts can paralyze spastic muscles effectively. Your doctor will determine the injection site based on the pattern of your spasticity.
When the doctor injects Botox into your muscles, it blocks the release of acetylcholine and leads to the relaxation of your overactive muscles. It can take several days for the injection to take effect and will last around 12 to 16 weeks until the growth of new nerve endings occurs, and your affected muscles recover. You may experience longer-lasting functional benefits.
Side effects of Botox are rare, but include excessive weakness in the site of the injection and weakness in adjacent muscles.
Selective dorsal rhizotomy (SDR) and intrathecal baclofen (ITB) are the main neurosurgical procedures for treating spasticity.
Some recent developments involving spasticity and clinical trials are:
To date, more than 800 clinical trials involving spasticity have been begun, abandoned or completed.
Research on THC, one of the main cannabinoids in medical cannabis, shows THC helps improve spasticity in MS patients, according to a study published in The Lancet. The endocannabinoid system takes up the THC and blocks lesion inflammatory action and improves communication between muscles and nerves. Also, since it reduces the inflammation, marijuana doesn’t just control pain, it also helps protect against further nerve degeneration which slows the progression of the disease.
Clinical trials of medical marijuana on spasticity in MS sufferers have shown mixed results. In one trial, subjective perception of muscle spasticity decreased in the sufferers, but observers saw no significant decrease and found it further impaired coordination. Another study showed a marked decline in spasticity. However, this was not a blind study. One study involving a single patient showed nabilone — synthetic THC — decreased spasticity.
These limited findings are consistent with what other medical marijuana research has found about the drug’s effects on the body. There is significant evidence medical marijuana can affect the central nervous system, which is where much spasticity originates. The endocannabinoid system is virtually everywhere in the human body. Therefore, it is not a leap to suggest medical marijuana can affect not only the root of the problem but also the spastic area in sufferers with nervous system disorders like MS.
MS gets the most attention when it comes to spasticity. However, spinal cord injury is another leading cause of muscle spasticity. It is also another area of medical marijuana research. Like MS, spinal cord injury can cause pain you can treat with medical marijuana. It is also possible to treat the spasticity in spinal cord injury with Sativa strains and their derivatives.
Also like MS, spinal cord injury sufferers will most often need long-term medical care. Therefore, individuals need safe alternatives to sedatives and traditional pain relievers for these conditions. Medical marijuana is showing promise in this area as well.
A double-blind study of a paraplegic spinal cord injury sufferer showed muscle spasticity decreased when the patient received THC. Furthermore, it worked better than the codeine the patient was receiving. This indicates medical marijuana is not only a viable treatment but may also be more successful in some patients than existing treatments. Nonetheless, more research is certainly necessary, as one patient cannot show how prevalent relief is among sufferers who received medical marijuana.
As with other conditions treated with medical marijuana, the anecdotal evidence that it works is staggering. One study showed nearly all of 112 survey respondents with multiple sclerosis had fewer incidences of muscle spasticity when taking marijuana. Another study of subjective sensations showed nearly half experienced less spasticity when on medical marijuana.
This is not overwhelming proof. However, it certainly suggests medical marijuana can increase the quality of life in many spasticity suffers. It also indicates in-depth and solid research into the treatment of spasticity with medical marijuana is vital. Safe, effective and tested medications are always essential for chronic conditions such as spasticity. Until there is a way to cure the damage leading to spasticity in most patients, the medical community must explore all avenues of relief for these sufferers.
Symptoms of medical marijuana and spasticity treatment can help with include:
Evidence shows pure CBD oral cannabis extract (OCE) drugs help reduce patients’ spasticity short-term, reports the American Academy of Neurology. THC oral spray and pills also help reduce spasticity in patients short-term. It reduces painful spasms and cramp-like pain. If patients continue taking them for at least a year, THC pills and OCE pills could continue reducing their spasticity.
THC pills and OCE pills can help reduce feelings of “pins and needles,” burning and numbness and help reduce frequent urination, according to research.
Side effects of marijuana can include dry mouth, red eyes, panic, impaired motor coordination, giddiness, increased heart rate and drowsiness.
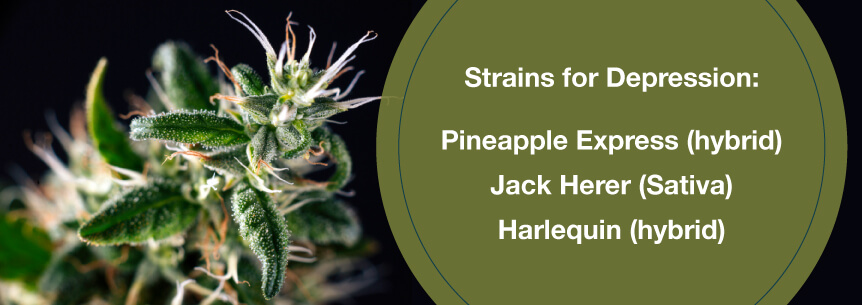
Finding the best marijuana for spasticity strains could take a little experimenting and guidance from a cannabis doctor. The doctor will use your symptoms, medical history, and disease progression to determine which strain or strains will best treat your symptoms. Some strains effective in treating MS symptoms, including muscle spasms and spasticity are:
Marijuana and spasticity treatment can make the perfect alternative to prescription drugs, which often have adverse side effects and addictive properties. Medical weed can also provide you with a better quality of life.
Some delivery methods of treatment include:
All of these methods may be helpful for spasticity. However, be advised smoking marijuana can cause respiratory issues, so choosing edibles, topicals or vaping may be better options for you.
For cannabis for spasticity treatment success, it’s essential you find a good dispensary and doctor. Find a qualified cannabis doctor here on MarijuanaDoctors.com to recommend your treatment. You can also connect with staff at a marijuana dispensary who can help point you in the right direction of which products and cannabis delivery methods will work for your symptoms.
If you’re suffering from spasticity and other symptoms and would like to know if medical cannabis will work for you, book an appointment with one of our highly trained and qualified cannabis doctors.
Find A Doctor Find A Dispensary