
Evidence supporting the assertion marijuana offers multiple medicinal properties for a whole range of disorders and diseases are increasing. Of all the research conducted on these many health conditions, the newest claim is that cannabis for type 2 diabetes is a potential treatment to help treat and prevent diabetes as well as the complications the disease causes.
Medical marijuana for type 2 diabetes is another option. Prevention of seizures, neurological pain and blindness can increase the quality of life in people with adult-onset diabetes. Medical marijuana is showing great potential in many of these areas. Furthermore, the components of marijuana some treatments do not produce psychoactive results. Therefore, it may eventually be considered for juvenile diabetes as well. Some forms of medical marijuana can increase hunger, and you should eat healthy foods if your appetite increases.
Find A Doctor Find A Dispensary
Given the nerve damage inherent in adult-onset diabetes, there is significant nerve pain in many cases. Nerve pain is one of the key areas of research regarding medical marijuana, and it is showing great promise. It has been shown to act as a pain reliever but is also known to alleviate neurological symptoms in incurable diseases like multiple sclerosis. It can also treat the pain of migraine headaches.
According to the Center for Medical Cannabis Research, medical marijuana trials showed that moderate doses of medical marijuana helped relieve nerve injury pain. HIV patients benefited from the increased appetite and decreased nausea caused by medical marijuana. They also appear to experience decreases in pain due to nervous system damage.
According to NORML, diabetic rats treated with medical marijuana showed reduced lack of oxygen delivery to the retina. Decreased oxygen to the retina is what causes blindness in diabetes. If this works in human trials, medical marijuana could prevent blindness in people diagnosed with Type 2 diabetes. Individuals who are taking medical marijuana to treat adult-onset diabetes could already be reaping this benefit.
On top of treating certain adult-onset diabetes symptoms, medical marijuana is also preventing diabetes in trials using mice. In the study, 86 percent of the mice who did not take cannabinoids got diabetes. Fifty-six percent fewer developed diabetes in those given cannabinoids.
It also seemed to stave off development of the disorder. Mice who took cannabinoids developed diabetes later than those who did not get cannabinoids, which is a good indication that cannabinoids can help prevent diabetes. However, it is unlikely that cannabinoids will be used as a preventative measure, though they may act as one if an at-risk patient takes them for another condition.
Some animal-based studies recently have shown a variety of health benefits with marijuana and type 2 diabetes treatment.
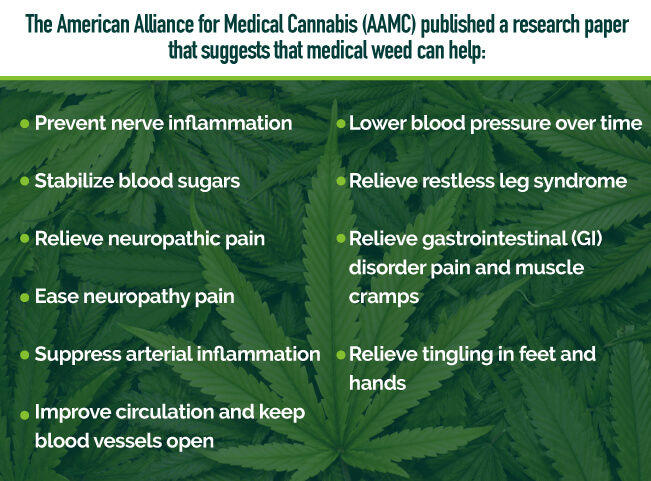
The American Alliance for Medical Cannabis (AAMC) published a research paper that suggests that medical weed can help:
Because this condition is complex and there’s still a lack of understanding, the benefits and drawbacks of marijuana for type 2 diabetes treatment in humans research is still in its early stages. On the other hand, animal studies have helped open doors for our understanding.
With the medical cannabis for type 2 diabetes industry expanding, doctors and patients look for useful ways to use this herb in treatment. The good news is there are other methods of use outside of smoking it. And, although many people still use traditional methods, they’re replacing these traditional methods with more high-tech and safer alternatives like:
With science evolving around cannabis and type 2 diabetes treatment and providing us with a better understanding of medical pot, more useful and safer methods are becoming more readily available.
Tetrahydrocannabinol (THC) is the main psychoactive in cannabis and helps ease discomfort and pain. However, cannabidiol (CBD) and tetrahydrocannabivarin (THCV), a lesser-known cannabinoid, both have anti-diabetic properties. Below are a handful of marijuana and type 2 diabetes strains that could prove beneficial.
Researchers say a complication that’s most common in diabetes is neuropathy, which is a dysfunction of your nerves. It’s one that’s most difficult to deal with and leads to pain, numbness and weakness.
Since medical weed has anti-inflammatory properties, it can help to eliminate nerve pain and heal damaged nerves. More specifically, the CBD is what’s “neuroprotective.” CBD can reduce neuropathic pain and protect the nerves from damage in patients with type 2 diabetes.
Because of this, the best diabetes cannabis strains are those that decrease diabetic neuropathic pain. The strains below are rich in antioxidant properties and high in CBD, therefore, protect your nerves and restores them. Some strains include:
There are more strains you can look for to help relieve your Type 2 Diabetes symptoms. These are only a handful. Search for a medical marijuana dispensary or doctor to find your perfect strain.
Find A Doctor Find A Dispensary
Diabetes is a chronic medical condition where your glucose (sugar) levels build up in your bloodstream. Insulin, a type of hormone, helps move the glucose into your cells from your blood for energy use. With type 2 diabetes, the cells of your body can’t respond to this insulin as they should. Doctors refer to as insulin resistance, particularly in the early onset of the mild form of the disease. Plus, your body might not make enough insulin in later stages of this disease.
Your pancreas produces insulin, and when you’re experiencing insulin resistance, your pancreas attempts to make even more insulin to get a response out of your cells. During this process, your pancreas eventually can’t keep up, raising your blood sugar and setting the groundwork for diabetes.
High blood glucose over time leads to issues like:
There are steps you can take to lower your risk of developing health issues related to diabetes.
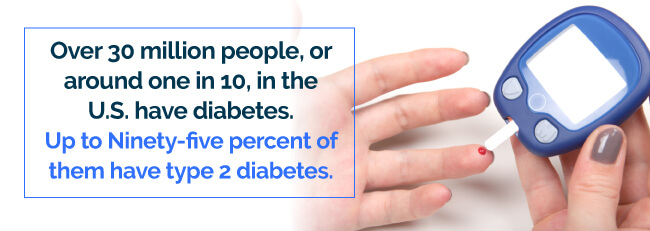
Over 30 million people, or around one in 10, in the U.S. have diabetes. Up to Ninety-five percent of them have type 2 diabetes. If you’re obese, older, don’t exercise or have a family history of the disease, the chances of you getting type 2 diabetes increases. Your risk also increases if you have prediabetes, which occurs when your blood glucose is higher than normal but isn’t high enough to be diabetes.
A combination of factors can cause the disease including having:
Other factors that put you at risk are due to your lifestyle choices and daily habits include:
These are risk factors you can control. And, since you can’t change what you’ve done in the past, moving forward, you’ll want to focus on the things you do have control over. For example, you can follow your physician’s recommendations to be healthy, take medication your doctor prescribes to you and even make small and simple positive changes on your own at home to manage your risk factors.
Your doctor can give you a blood test to see if you have diabetes. You may even go to a pharmacy or health clinic to check your blood sugar, but be sure you follow up with your doctor to make sure you received accurate results.
For thousands of years, diabetes has been making an impact on people’s lives. Egyptians acknowledged a condition they suspected was diabetes in manuscripts dating back to 1550 BCE. Ancient Indians in the Sixth Century B.C. E. also knew about the condition, according to The National Medical Journal of India.
The American Diabetes Association notes that medical professionals in 1910 were the first to take steps toward finding the cause of diabetes and devising a treatment approach.
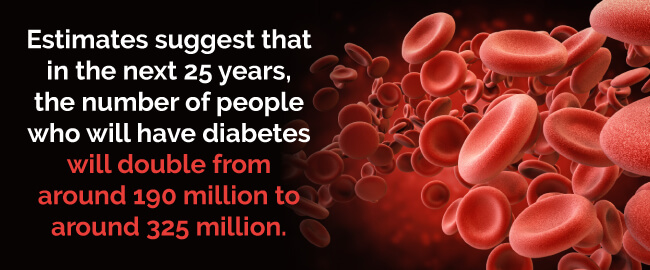
Type 2 diabetes is a dominating cause of individuals dying prematurely. Estimates suggest that in the next 25 years, the number of people who will have diabetes will double from around 190 million to around 325 million. But, being tested, receiving treatment and making changes in lifestyle choices— like eating healthy and exercising can help prevent diabetes and provide beneficial effects to people’s health. It’s also important to public health to promote adherence to these changes.
Type 2 diabetes may come on gradually. You can experience both physical and mental effects of the disease:
Your symptoms might be mild enough that you may dismiss them at first. Some early symptoms could include:
As your diabetes progresses, however, your symptoms could become more severe. If your blood glucose levels are high for an extended period, your symptoms can become potentially dangerous. You may experience:
See your physician if you experience any of these symptoms. Type 2 diabetes can turn life-threatening without treatment.
Long-term complications of diabetes include:
Type 2 diabetes doesn’t just accompany physical effects. You may experience mental effects that you have to worry about as well.The Journal of the American Medical Association published a report online on that claimed that out of all the comorbidities linked to diabetes, the most overlooked are mental-health problems. Mental health issues have a tremendous potential of compromising your ability to self-manage your diabetes and increases your chances of getting serious complications.

Some potential mental-health issues related to diabetes are as follows.
Major depressive disorder affects 6.7 percent of American adults, and across a lifespan, the rates of this disorder are two times higher in people with type 2 diabetes. As researchers strive to get a better understanding of the components that link diabetes and depression, they’ve concluded that their relationship is bidirectional. That is, when you have depression, your risk for diabetes increases, just as having diabetes increases your risk of depression.
According to the JAMA report, depression isn’t the only mental-health effect linked with diabetes. Anxiety, panic disorder and posttraumatic stress disorder are just as probable in people with diabetes whether or not they have depression.
Also, since symptoms of anxiety may overlap hypoglycemia symptoms, diabetic patients don’t know if the cause is low blood glucose, which requires treatment immediately, or not. Not to mention, when patients are struggling with anxiety over this confusion, they may over-treat themselves that leads to blood sugar being higher than target levels.
Although there isn’t abundant information about diabetic males with eating disorders, research shows it’s a significant issue in diabetic women. Compared to people without type 2 diabetes, those with the disease have double the risk of getting a full-blown eating disorder along with a 1.9-fold chance of getting a sub-threshold eating disorder.
And, like other mental-health disorders, eating disorders can cause an overflow of complications and the disease can become worse since eating behaviors that are disordered can persist and get worse over time.
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIH):
A 2017 National Diabetes Statistics Report estimates that:
There are some medications aimed at treating diabetes, its symptoms and diabetes complications. Treatment emphasizes maintaining normal blood sugar levels, having a healthy diet and getting sufficient exercise. However, several levels of treatment and prevention must be considered and studied.
Type 2 diabetes treatment mainly consists of monitoring your blood glucose, insulin, taking diabetes medications or both.
Many individuals who have type 2 diabetes require insulin treatment. Types of insulin that include:
Your physician may prescribe a combination of insulin types to use during the day and at night, depending on your needs.
Low blood sugar, or hypoglycemia, is the main side effect of insulin. Other side effects may include:
In some cases, doctors may prescribe injected or oral medications. Some of these types of medication stimulate your pancreas to make more insulin and release it. Other types work by inhibiting glucose production and release from your liver so your body can move glucose into your cells with less insulin.
Other types of medications cause your tissues to become insulin sensitive or block stomach action or intestinal enzymes that break your carbohydrates down. Doctors typically prescribe metformin first as a type 2 diabetes treatment.
Potential diabetes medication side effects may include:
Always consult with your physician for possible side effects of diabetes medication since lists of side effects could be incomplete.
Bariatric surgery isn’t necessarily a type 2 diabetes treatment. However, if have type 2 diabetes and have a 35 or more body mass index, you could benefit from this particular surgery. It’s shown blood glucose level improvements in people who had this surgery.
Potential side effects of bariatric surgery include:
Certain lifestyle and diet changes can be beneficial such as:
Eating healthy: There isn’t a particular diet for diabetes. However, you should include more whole grains, fruits and vegetables in your diet. Your food should be low in calories and fat and high in nutrition. Cut back on refined carbohydrates, animal products and sweets.
Depending on the severity of your diabetes, it may be okay to consume sugary foods once in awhile, but only if you count them as part of your meal plan and if approved by your doctor. You may want to consult with a registered dietitian who can help you come up with a meal plan that meets your food preferences, health goals and lifestyle.
Exercise or physical activity: All people need to be physically active on a regular basis, even diabetics. Physical activity, particularly exercise and workouts move glucose into your cells using it for energy and lowering your blood glucose level. Exercise also raises your insulin sensitivity causing your body to require less insulin to move the glucose into your cells.
Once your physician approves you exercising, you can pick physical activities you enjoy like swimming, walking or biking. Try to include exercise or other physical activities into your everyday routine aiming for a minimum of 30 minutes daily several days a week. Start off slow if you’re just beginning to get active and gradually build up.


Please allow us to access your location to find local dispensaries.
VIEW ALL DISPENSARIES ➔